The digitization of pathology slides and the adoption of the DICOM (Digital Imaging and Communications in Medicine) format are profoundly transforming the medical landscape, offering innovative and standardization prospects in the field of digital pathology. This evolution has been driven by the constant search for more effective ways to visualize, share, and interpret pathological images, paving the way for a better understanding of pathologies and more personalized care.
The transformation of Pathological Anatomy and Cytology (PAC) towards digitized virtual slides represents a significant advance. Virtual slides, which are high-resolution digital representations of pathological tissue samples, are a valuable alternative to traditional microscopy. To fully grasp this transition, it is necessary to examine in depth the issues related to slide digitization and to understand the fundamental role played by the DICOM format in this context.

The challenges of digitizing pathology slides
What is a digital slide?
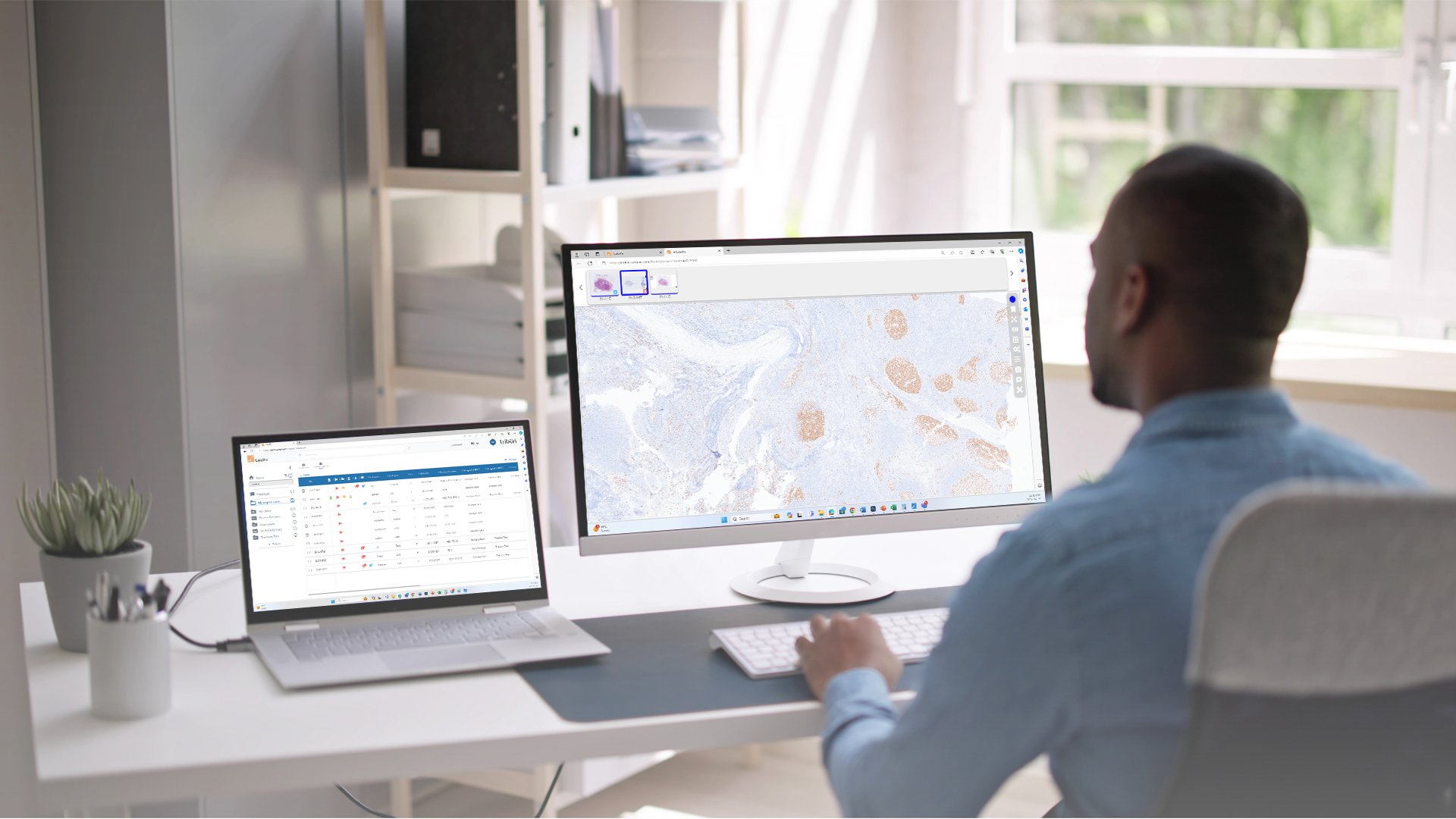
 Whole Slide Images (WSI) are high-resolution digital representations of a pathology tissue sample obtained by scanning. They are digitized by slide scanners that, composed of a microscope objective, a motorized stage, and a camera, allow the generation of a digital facsimile of the glass slide in one minute. There are about ten slide scanner manufacturers worldwide. The main ones in Europe and North America are Hamamatsu, Leica, 3D Histech, and Philips.
Whole Slide Images (WSI) are high-resolution digital representations of a pathology tissue sample obtained by scanning. They are digitized by slide scanners that, composed of a microscope objective, a motorized stage, and a camera, allow the generation of a digital facsimile of the glass slide in one minute. There are about ten slide scanner manufacturers worldwide. The main ones in Europe and North America are Hamamatsu, Leica, 3D Histech, and Philips.
According to a study in the "Journal of Pathology Informatics," digitized slides offer detailed visualization of tissues at the cellular level due to their high image resolution and simplified digital navigation. By eliminating the need for physical handling, these slides facilitate digital storage, sharing, and provide interactive features. Automated analysis and the ability to remotely access data enhance their accuracy and practicality, making them an advanced alternative to traditional microscopy for medical research.
Digitization poses new challenges, particularly with regard to the read format and management of slide storage. Indeed, a digital slide is represented by a high-resolution file of several tens of thousands of pixels, with a size ranging from a few hundred MB to a few GB. On average, each digital slide reaches a size of 1.3 GB. These image files are therefore very large, far exceeding the requirements of traditional radiological exams. This raises the question of appropriate formats for reading, visualizing, sharing, and storing these digitized slides.
What are the existing formats for reading a digitized slide?
All slide manufacturers have developed a proprietary format for creating their images. Various formats such as JPEG, PNG, and TIFF are frequently used for viewing digitized slides. These exclusive formats are all based on a tiled and pyramidal architecture. The tiles are encoded in JPG, which means that no virtual slide is free from compression, and they are organized in a pyramidal structure. This implies that multiple zoom levels are recorded, thus allowing for quick access during consultation. However, this pyramidal structure results in approximately 30% information redundancy in each file.
To view these slides, different viewers have integrated the ability to read these proprietary formats natively. This integration was done either by integrating APIs provided by the manufacturers, or by developing the technical specifications of the different formats, or by using a partial open source library OpenSlide. These proprietary formats are generally very efficient both in terms of scanning and visualization, which explains why they are today very widely used.
This performance is due to the investments made by the industry on the one hand and to the choice of a tiled and pyramidal structure, particularly well suited to navigation in a very large image. However, these formats do not always meet medical standards. According to the "Journal of Digital Imaging" (Pianykh, 2018), the use of non-standardized formats can lead to interoperability and image quality problems. The alternatives, including JP2, have all been abandoned. The need for a standardized format is therefore more necessary than ever.

DICOM: a standard format for managing and transmitting medical images
The Birth of DICOM in Pathology
In 2006, a dedicated DICOM group in pathology was created thanks to a Franco-American initiative, with France represented by Adicap and Jacques Klossa, a member of the Tribun Health administration committee, as the first European co-chair. This group, the WG26 of Nema, quickly published two technical guides (TF 122 and 145) on the encoding of Whole Slide Images (WSI) in DICOM and on the associated data schema.
It is essential to note that DICOM is not limited to being simply an image format; it also encompasses a structuring of associated data and is a communication protocol between the three major components of the imaging chain: modality, visualization, and storage. For example, in the field of radiology, this concerns the scanner, the radiologist's station, and the Picture Archiving and Communication System (PACS).
DICOM, initially designed for radiology, has been extended to pathology to meet the growing needs for standardization of medical images. According to a publication in the European Journal of Radiology (Carriero et al., 2020), this extension was motivated by the need for uniform management of pathological data, thus facilitating seamless integration into existing health systems. In other words, this extension of DICOM to pathology aims to ensure optimal interoperability between the various medical modalities and to facilitate the integration of pathological data into existing health infrastructures.
A belated adoption...
The late adoption of DICOM in pathology can be explained by various factors that have limited its implementation by industrial players, whether scanner vendors, software publishers or storage infrastructures. These reasons include technical aspects, such as the initial management of intellectual property and patent issues, the historical inability of the Task Force (TF) to handle fluorescence and z-stack, and the management of large quantities of annotations from artificial intelligence.
Performance considerations also contributed, notably due to the greater weight of DICOM files and their slowness compared with native formats. Economics, such as implementation cost and lack of solvent customer demand, also played a role, as did ecosystem considerations - the adoption of DICOM may seem of little use if other components in the imaging chain are not compatible.
 As a result, DICOM implementations in pathology have mainly been limited to research or marketing purposes, often in the form of products derived from native formats. Furthermore, in cases where scanners do not produce natively in DICOM, the transformation of native format images into DICOM format (secondary dicomization) has significantly complicated the workflow in terms of time and data volume, making this approach unfeasible in production scenarios.
As a result, DICOM implementations in pathology have mainly been limited to research or marketing purposes, often in the form of products derived from native formats. Furthermore, in cases where scanners do not produce natively in DICOM, the transformation of native format images into DICOM format (secondary dicomization) has significantly complicated the workflow in terms of time and data volume, making this approach unfeasible in production scenarios.
To overcome these obstacles, the "DICOMPathology" project, detailed in a study by Clunie et al. (2018), played a key role in providing specific guidelines for the successful integration of DICOM in pathology. These guidelines addressed technical aspects, such as fluorescence management, and aligned DICOM with the unique needs of pathology. By focusing on interoperability, the project contributed to a change in attitude, facilitating the adoption of DICOM in the pathology community and overcoming previous obstacles.
Standardization is necessary and unavoidable
Current dynamics point to rapid change, anticipating that DICOM will become the norm in the next few years. The widespread adoption of digital pathology is profoundly transforming the medical landscape, making standardization essential. This necessity is accentuated by the growing role of medical information systems (IMS), which have become decisive players, implementing institutional strategies centered on data, notably images, that require interoperable standards. This is crucial for patient records, multimodal artificial intelligence and, of course, archiving.
As a result, most establishments are moving towards the implementation of global image storage and archiving solutions, using on-site servers or VNA (Vendor Neutral Archive) cloud solutions. These VNAs are designed specifically for DICOM formats and protocols. Pathology, alongside radiology, genomics and cardiology, now occupies a central place, a position it has never held in traditional PACS. The implementation of these standardized, neutral image infrastructures opens up significant prospects for the digital transition of Pathological Anatomy and Cytology (PAC).
The adoption of DICOM in pathology offers major advantages. According to the American Journal of Clinical Pathology (O'Neill et al., 2021), the use of DICOM facilitates more accurate interpretation of pathology images, enhancing diagnostic reproducibility and contributing to substantial improvements in patient care.
The importance of industrial investment in the interests of customers and patients
The current state of DICOM integration with existing systems
Despite some progress, major industrial investment is still required along the chain to guarantee coverage and functional performance equivalent to existing proprietary formats. Some scanners, such as Leica and Hamamatsu, have begun integrating the native production of DICOM files, while some editors, notably Tribun Health since July 2023, are now able to manage DICOM images. At the same time, VNA suppliers such as GE Healthcare and Canon are working on the necessary communication and archiving protocols.
In the context of regional projects, it is strongly recommended that DICOM be adopted with determination, particularly in the area of archiving. Large-scale projects, with their funding capacity, are essential drivers for advancing solutions, in the interests of both customers and patients.
Significant investments in DICOM integration play a critical role in the transition to digital pathology practices. According to a study conducted by Healthcare Information Management & Communications Canada (HIMCC, 2019), successful integration improves the operational efficiency of pathology laboratories by simplifying workflows and fostering better interdisciplinary collaboration.
Accessibility and availability of medical data
Investment in DICOM integration plays a central role in improving accessibility to digitized medical data, offering significant benefits for patient care and collaboration between healthcare professionals.
DICOM, as a standard, is making a significant contribution to the increased accessibility of medical data. According to research published in "JAMA Network Open" (Mukhopadhyay et al., 2020), the use of DICOM facilitates search and access to pathological images. This ease of access accelerates the clinical decision-making process, enabling practitioners to quickly obtain crucial information for faster, more accurate patient management.
The impact of this increased accessibility is not limited to faster decision-making. It also promotes closer collaboration between healthcare professionals. The DICOM standard enables efficient data sharing between different medical departments, contributing to smoother coordination and better understanding of complex clinical cases. This translates into a significant improvement in the quality of care, as medical teams can collaborate more effectively, share relevant information and develop more coherent treatment strategies.
Data security and confidentiality
In addition, the DICOM format secures data primarily through the implementation of security protocols, with particular emphasis on data encryption. DICOM data encryption involves converting medical information into a code that cannot be read without the appropriate decryption key. This creates an effective barrier against unauthorized access, guaranteeing the confidentiality of medical records.
In short, the DICOM format plays an essential role in securing medical data, underlining its positive impact on confidentiality, stakeholder confidence and quality of care.

Conclusion
In conclusion, the digitization of pathology slides and the adoption of the DICOM format are crucial for the future evolution of medical practices. The transition to digital slides enables healthcare professionals to collaboratively access high-resolution images, transcending the traditional limits of microscopy. The need for a common standard for the visualization and management of pathology images is highlighted by the challenges associated with slide digitization. DICOM is the only sustainable pathway to standardization, despite an initially slow adoption due to the specificities of pathological workflows.
Industrial investments in the integration of DICOM with existing systems are continually improving the operational efficiency of pathology labs, ensuring a smooth transition to digital practices. Increased accessibility to medical data through DICOM accelerates the clinical decision-making process, offering tangible benefits in terms of patient care quality. The security measures built into DICOM reaffirm the commitment to the privacy of sensitive medical data, strengthening patient and healthcare professional trust in the use of this technology.
In a constantly evolving medical landscape, it is imperative to advance in the digitization of ACP and the adoption of the DICOM format. These advancements represent a significant step towards a more precise, collaborative, and efficient diagnostic practice, offering considerable potential to improve patient care and redefine the way medical information is managed and shared in the field of pathology.

Sources
- Implementing the DICOM Standard for Digital Pathology; J Pathol Inform. 2018; 9: 37. Published online 2018 Nov 2. doi: 10.4103/jpi.jpi_42_18
- DICOM Whole Slide Imaging (WSI) https://dicom.nema.org/dicom/dicomwsi/
- Smith, A. R., & Weinstein, R. S. (2019). "The evolution of pathology informatics terminology and concepts: What is a 'Lame' and what does it mean?". Journal of Pathology Informatics, 10, 4. doi:10.4103/jpi.jpi_54_18
- Pianykh, O. S. (2018). "Digital Imaging and Communications in Medicine (DICOM) in pathology". Journal of Digital Imaging, 31(3), 283-291. doi:10.1007/s10278-017-0011-9
- Carriero, A., & De Silva, T. (2020). "DICOM in Pathology: History, Current and Future Status". European Journal of Radiology, 122, 108760. doi:10.1016/j.ejrad.2019.11.024
- Clunie, D. A., et al. (2018). "DICOM pathology supplement 145: Whole slide microscopic image IOD and SOP Classes". Journal of Digital Imaging, 31(3), 324-333. doi:10.1007/s10278-018-0080-7
- Healthcare Information Management & Communications Canada (HIMCC) (2019). "DICOM interoperability: The essential element for a connected digital health system". HIMCC
- Mukhopadhyay, S., et al. (2020). "Whole Slide Imaging Versus Microscopy for Primary Diagnosis in Surgical Pathology: A Multicenter Blinded Randomized Noninferiority Study of 1992 Cases (Pivotal Study)". American Journal of Surgical Pathology, 44(2), 285-292. doi:10.1097/PAS.0000000000001432
- Kamal, R., et al. (2021). "An investigation of security vulnerabilities in DICOM networks". Journal of Digital Imaging, 34(4), 778-784. doi:10.1007/s10278-021-00473-w





.png?width=256&height=256&name=customer-service(1).png)



.png?width=64&height=64&name=calendrier(1).png)
.png?width=64&height=64&name=communique-de-presse(1).png)
.png?width=64&height=64&name=livre(1).png)
.png?width=64&height=64&name=blog(2).png)