HER2 grading is a key factor in the diagnosis and treatment of breast cancer. It determines eligibility for targeted therapies that can block tumor growth effectively. This article explores traditional methods for determining HER2 status, the challenges faced by pathologists, and the contribution of artificial intelligence (AI) in enhancing the accuracy and reproducibility of diagnosis.
What is HER2 Grading and Why it is Important?
HER2 grading assesses the presence and levels of the HER2 protein (Human Epidermal Growth Factor Receptor 2) in tumor cells. When this protein is overexpressed, it can lead to rapid and aggressive tumor growth.
Targeted treatments, such as HER2 inhibitors, specifically block the HER2 protein, halting the proliferation of cancer cells. Initially, these therapies were limited to patients with high HER2 expression (3+ score). However, recent clinical trials indicate that treatment is also beneficial for patients with low or very low HER2 expression (low HER2 or ultra-low HER2).
As a result, patients with minimal HER2 expression can also benefit from targeted therapies. This precise targeting spares patients many of the side effects associated with traditional chemotherapy, which affects both healthy and cancerous cells.
It is therefore crucial to accurately determine the level of HER2 protein expression for the diagnosis of breast cancer. 
Determining HER2 Grading: Techniques and Evaluation Criteria
1. Criteria for HER2 Grading
To determine whether a tumor is HER2-positive or negative, pathologists use a classification system based on the intensity and localization of HER2 staining observed during immunohistochemistry (IHC) tests. The results are classified as follows:
- 0 : No staining or weak staining in less than 10% of cells, considered HER2-negative.
- 0+: Weak staining in more than 1% of cells, considered HER2 ultra-low.
- 1+: Weak staining in 1% to 10% of cells, considered HER2 low.
- 2+: Moderate staining in more than 10% of cells, considered HER2 ambiguous. This result requires a FISH (Fluorescence In Situ Hybridization) test to check for HER2 gene amplification. If amplification is present, the tumor is classified as HER2-positive.
- 3+: Intense staining in more than 10% of cells, considered HER2-positive.
2. Techniques for Determining HER2 Grading
- Immunohistochemistry (IHC) :
- The primary diagnostic tool for HER2 grading.
- Pathologists use a staining process to detect HER2 proteins, which appear as brown or red markings on cell membranes.
- In Situ Hybridization (FISH, CISH, SISH) :
- A molecular biology test used when IHC results are inconclusive (score 2+).
- Detects HER2 gene amplification, confirming whether the cancer is HER2-positive.
3. Challenges in Assessing HER2 Grading
Manual interpretation of HER2 grading presents several challenges :
- Variability among pathologists : The assessment by the pathologist's eye remains subjective, and determining expression thresholds (such as the 10% marked cell threshold) can sometimes be difficult.
- Differences in guidelines : Interpretation criteria may vary depending on recommendations from scientific societies, leading to discrepancies between laboratories.
- Sample quality : Tissue fixation can sometimes alter results, especially when comparing biopsy samples with surgical specimens.
- Interpretation of intermediate scores (1+ or 2+) : These cases often require additional tests, which can delay the diagnosis.

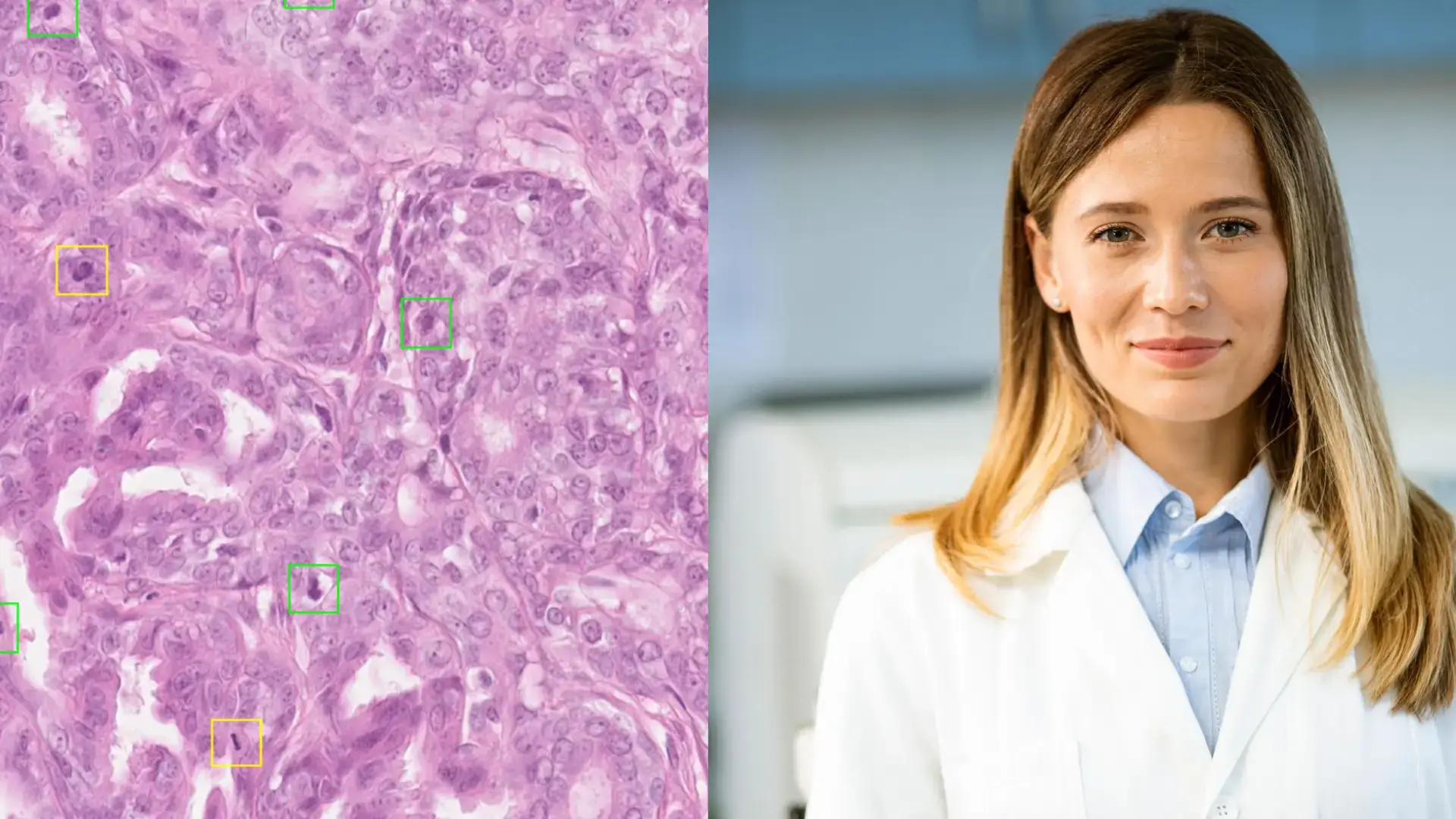
Artificial Intelligence in HER2 Grading Assessment
There are many compelling reasons to use digital pathology to overcome the challenges associated with HER2 grading assessment. Although these digital tools are not yet widely used in routine practice, current applications show several advantages:
1. Improvement in Reproducibility
Beyond accuracy, AI enhances the reproducibility of HER2 grading assessments. With deep learning algorithms, AI can analyze digital images of slides more objectively and consistently than the human eye. Each slide is segmented into small tiles, allowing the algorithm to scrutinize each area and analyze the staining and appearance of cell membranes.
This overcomes human biases (fatigue, lighting variability, etc.) and provides a more stable diagnosis, particularly in cases where scores are close to thresholds (e.g., between 0 and 1+). AI can accurately calculate the percentage of marked cells and standardize results across different laboratories.
2. Reduction of Ambiguities in Intermediate HER2Grading
In cases where HER2 Grading presents an uncertain score, particularly for 2+ results requiring FISH tests, AI can help reduce ambiguities by detecting positive cells more quickly and accurately. This could, in some instances, avoid additional examinations and thus accelerate diagnosis timelines. However, internal validation of the algorithm by laboratories is crucial to ensure this effectiveness.
3. Increased Precision in Analyzing Cell Staining
If well-calibrated, the algorithm can also offer increased precision in counting marked cells, particularly in borderline cases. Unlike human analysis, AI is not limited by subjective criteria and can count each cell meticulously. This capability of AI could be particularly useful for establishing a low or ultra-low HER2 grading.
4. Workflow Optimization and Training
Despite these benefits, integrating AI into daily practice presents challenges, particularly regarding costs and adaptation to existing laboratory workflows. A digital transformation will also need to occur. Pathologists will need specific training to use these tools effectively. Furthermore, the chosen algorithm must be carefully validated internally to ensure its reliability compared to traditional methods.
AI and HER2 Grading Diagnosis: Future Perspectives
In the long term, AI could fundamentally transform pathology practice, including HER2 status classification. With proper training and rigorous validation, these technologies can provide improved precision, reproducibility, and diagnostic quality while accelerating patient care processes. For difficult-to-determine scores, such as low and ultra-low, AI could have a significant impact. Over time, AI may not only assist pathologists but also potentially automate certain diagnostic steps entirely.
Conclusion
In conclusion, AI through diagnostic support algorithms, promises to significantly improve HER2 status evaluation. Breast cancer diagnostics are heading toward greater automation, enabling standardized practices, faster and more reproducible diagnoses, and ultimately better patient care.
Contact us today to experience a live demo of Tribun Health’s platform and see how our end-to-end solution and AI tools can transform your lab’s workflow.




.png?width=256&height=256&name=customer-service(1).png)



.png?width=64&height=64&name=calendrier(1).png)
.png?width=64&height=64&name=communique-de-presse(1).png)
.png?width=64&height=64&name=livre(1).png)
.png?width=64&height=64&name=blog(2).png)